
BREAKING NEWS…
We would like to invite you to an afternoon seminar by one of our Visiting Faculty, Professor Mike Wee, presenting some exciting new research findings to come out of a recently completed Research for Patient Benefit funded study comparing two methods of pain relief during labour (abstract and biography below). This paper was just voted best paper of the conference at the Obstetric Anaesthetists Association Annual Conference in Liverpool and was featured recently in the Bournemouth Echo http://www.bournemouthecho.co.uk/news/9770928.Pain_relief_in_labour__study_at_Poole_hospital_makes_important_discovery/
The seminar is scheduled for Thursday 19th July 2-3pm in BG10 Bournemouth House (after the HSC end of term lunch and next door for your convenience).
We hope you can make it and look forward to seeing you then.
BUCRU
Website: http://microsites.bournemouth.ac.uk/bucru/
Administrator: +44 (0)1202 961939 / wardl@bournemouth.ac.uk
Title: The IDvIP Trial: A two-centre double blind randomised controlled trial comparing i.m. diamorphine and i.m. pethidine for labour analgesia
Research team and affiliations: MYK Wee, JP Tuckey,* P Thomas,† S Burnard,* D Jackson.
Poole Hospital NHS Foundation Trust, Poole, UK, *Royal United Hospital, Bath, UK, †Bournemouth University Clinical Research Unit, Bournemouth, UK.
Abstract:
Background: Intramuscular pethidine, the commonest parenteral opioid analgesic used in obstetrics and more recently diamorphine usage has increased in the UK. The maternal, fetal and neonatal side effects are well known for pethidine but there are no sufficiently powered large RCTs comparing pethidine with diamorphine. The aim of this trial is to address this.
Methods: After ethical approval, informed consent was obtained from 484 women randomised to receive either 7.5mg diamorphine i.m. or 150mg pethidine i.m. for labour analgesia. The sample size calculation derived from a small RCT giving 90% power (at the 5% significance level) is based upon the maternal primary outcome measure of pain relief at 60mins and the neonatal primary outcome measures of Apgar Score of <7 at 1min and neonatal resuscitation. Secondary outcome measures include verbal pain intensity at 60mins and over 3hrs post-analgesia, pain relief over first 3hrs, maternal oxygen saturation, sedation, nausea and vomiting and maternal satisfaction with analgesia. Fetal and neonatal secondary outcomes include CTG trace, meconium staining, UApH, UVpH, time of delivery to first breath, Apgar Score at 5mins, naloxone use, neonatal oxygen saturations, sedation and feeding behaviour for the first 2hrs after delivery.
Results: Reported using CONSORT guidelines. At 60mins post-administration and over a 3hr period, diamorphine is better at reducing pain scores than pethidine (p<0.001). There were no statistical differences between the two groups regarding Apgar Scores of <7 at 1min and the need for neonatal resuscitation. The time between first dose administered and delivery is on average 82mins longer with the diamorphine group compared to pethidine (p<0.001). The vast majority of women experienced moderate to severe pain at all times. Women receiving diamorphine were more satisfied with their analgesia. There were no statistically significant differences in maternal sedation, nausea and vomiting or oxygen saturations over the 3hr period. There were no statistically significant differences in the fetal and neonatal outcomes including feeding behaviour between the two groups within 2hrs of birth but neonates in the pethidine group were more likely to be moderately or severely sedated at delivery.
Discussion: Intramuscular 7.5mg diamorphine gives significantly better analgesia than 150mg pethidine but prolongs delivery by approx. 82mins. Women given diamorphine are more likely to be satisfied with their analgesia. The mechanism for the prolongation of delivery time in the diamorphine group should be investigated further.
Acknowledgement: This research was funded by the NIHR Research for Patient Benefit Programme (PB-PG-0407-13170).
References
1. Tuckey JP, Prout RE, Wee MYK. Prescribing intramuscular opioids for labour analgesia in consultant-led maternity units: a survey of UK practice. International Journal of Obstetric Anesthesia 2008, 17(1):3-8.
2. Fairlie FM, Marshall L, Walker JJ et al. Intramuscular opioids for maternal pain relief for labour: a randomised controlled trial comparing pethidine with diamorphine. British Journal of Obstetrics and Gynaecology 1999; 106(11): 1181 -1187.
Biography of speaker:
Michael Wee is a consultant anaesthetist from Poole Hospital and Royal Bournemouth Hospitals. He has a special interest in obstetric anaesthesia and is the lead obstetric anaesthetist at Poole Hospital. He is chair of the Research and Innovations Group at Poole Hospital and is a Board member of the Western Comprehensive Local Research Network. He was awarded a visiting professorship at Bournemouth University in 2009. He is a referee for several medical journals. His research interests include patient information, safety in anaesthesia, maternal analgesia and simulation in epidural anaesthesia. He is a co-supervisor of a PhD student at BU and chief investigator of the MObs study investigating early warning scores in obstetrics.
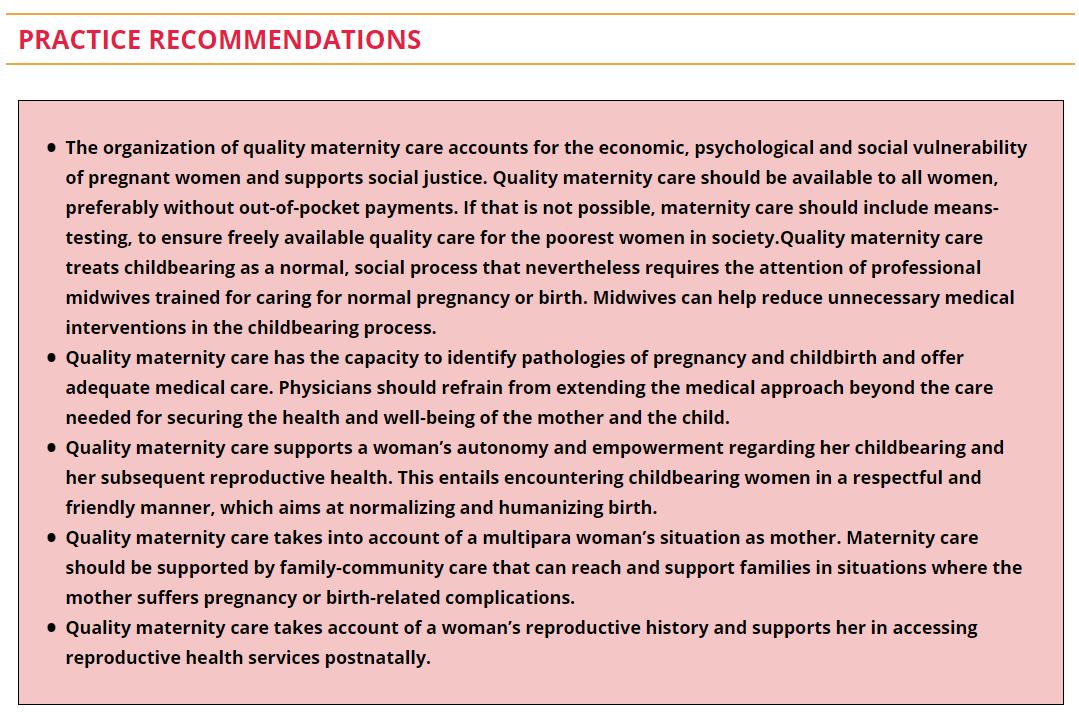
 Congratulations to Bournemouth University’s PhD student Sulochana Dhakal-Rai on the publication today of the latest paper from her research thesis. This latest paper ‘Factors contributing to rising cesarean section rates in South Asian countries: A systematic review‘ has been published in the Asian Journal of Medical Sciences [1].
Congratulations to Bournemouth University’s PhD student Sulochana Dhakal-Rai on the publication today of the latest paper from her research thesis. This latest paper ‘Factors contributing to rising cesarean section rates in South Asian countries: A systematic review‘ has been published in the Asian Journal of Medical Sciences [1]. The paper is part of her PhD study of the rising CS rate in Nepal. This systematic review is co-authored with her BU PhD supervisors, Dr. Juliet Wood, Dr. Pramod Regmi and Prof. Edwin van Teijlingen as well as her Nepal-based supervisors Dr. Ganesh Dangel (FHSS Visiting Faculty) and Dr. Keshar Bahadur Dhakal. This is the sixth paper from Sulochana’s interesting and highly topical PhD thesis. The previous five were published in 2018, 2019 and 2021 [2-6].
The paper is part of her PhD study of the rising CS rate in Nepal. This systematic review is co-authored with her BU PhD supervisors, Dr. Juliet Wood, Dr. Pramod Regmi and Prof. Edwin van Teijlingen as well as her Nepal-based supervisors Dr. Ganesh Dangel (FHSS Visiting Faculty) and Dr. Keshar Bahadur Dhakal. This is the sixth paper from Sulochana’s interesting and highly topical PhD thesis. The previous five were published in 2018, 2019 and 2021 [2-6].



















 Upcoming opportunities for PGRs – collaborate externally
Upcoming opportunities for PGRs – collaborate externally BU involved in new MRF dissemination grant
BU involved in new MRF dissemination grant New COVID-19 publication
New COVID-19 publication Conversation article: London Marathon – how visually impaired people run
Conversation article: London Marathon – how visually impaired people run MSCA Postdoctoral Fellowships 2024
MSCA Postdoctoral Fellowships 2024 Horizon Europe News – December 2023
Horizon Europe News – December 2023