by Prof Sam Porter, Chair of the Science, Technology & Health Research Ethics Panel
 One of the core principles of ethical research is that people should have a free choice as to whether or not they wish to participate in a research project, and that they should know what that will involve and how it might affect them before they make that choice. In short, they should give their informed consent. What we wish to concentrate on in this blog is the ‘informed’ bit of this phrase. In our work on ethics panels, we have sometimes observed applications in which almost all the concentration is on the ‘consent’ part, making sure that the paperwork giving permission to proceed is correct and watertight. This is unfortunate, because if someone is not properly aware of what they are letting themselves in for, then their consent is meaningless; it is ‘uninformed‘. This isn’t a matter of researchers deliberately setting out to hoodwink and deceive potential participants; it’s more a matter of them pitching the information at a level that compromises clarity and ease of understanding.
One of the core principles of ethical research is that people should have a free choice as to whether or not they wish to participate in a research project, and that they should know what that will involve and how it might affect them before they make that choice. In short, they should give their informed consent. What we wish to concentrate on in this blog is the ‘informed’ bit of this phrase. In our work on ethics panels, we have sometimes observed applications in which almost all the concentration is on the ‘consent’ part, making sure that the paperwork giving permission to proceed is correct and watertight. This is unfortunate, because if someone is not properly aware of what they are letting themselves in for, then their consent is meaningless; it is ‘uninformed‘. This isn’t a matter of researchers deliberately setting out to hoodwink and deceive potential participants; it’s more a matter of them pitching the information at a level that compromises clarity and ease of understanding.
What we wish do here is to provide a few pointers that will help ensure that your Participant Information Sheet is written in a style that facilitates effective dissemination to potential participants of the information they require to make an informed decision.
- Avoid blinding by science: researchers can be so immersed in their research that the language of their subject area becomes so natural to them they assume that everyone shares that language. Rest assured that they do not. It is really important to avoid technical research terms in a Participant Information sheet and to describe what you are doing in language that will be understood by those not involved in your research speciality.
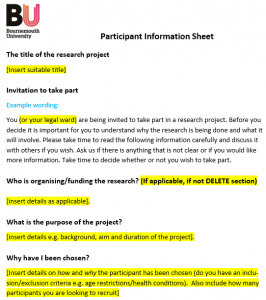
- Indeed, we would go farther than that. The language used in a Participant Information Sheet should be accessible to all those who are being asked to participate. Perhaps because they spend their working lives in tertiary educational environments, researchers tend to greatly overestimate people’s linguistic capacities. The US National Center for Biotechnical Information recommends that a patient information sheet should be pitched at a reading age of 11-12 years old. Indeed, this may not be young enough. There is evidence to indicate that the average adult reading age in the UK is 9 years old. Remember, this is an average which means lots of people have a younger reading age.
- Whatever you may think of its editorial line, you could do worse than model your language level on that of The Sun, which has a young reading age and adopts a clear, no nonsense, if sometimes overly aggressive style. While use of the active voice and a conversational tone is much more effective than passive formality, a Participant Information Sheet should always be polite, respectful and invitational in its approach.
- Pitching a Participant Information Sheet at a young reading age is not about being patronising but being clear. Indeed, the clarity that it demands is a very good exercise for researchers to make sure that, without the camouflage of technical jargon and convoluted language, their research project has a transparent logic and is practically cogent.
- Of course, one size does not fit all. For example, if you were conducting research into a health service organisation, it could be appropriate to include more professionally-oriented information in a Participant Information Sheet seeking to recruit senior health service managers than if members of the general public were being asked to be involved. Still, we would recommend always erring on the side of simplicity and clarity, rather than assuming knowledge that people may not have. If groups with different sorts of knowledge and perspectives are being asked to be involved, we would advise that separate, specifically targeted Information sheet should be used to inform the members of each group.
- You can check the reading level of your Participant Information Sheet on Word. We’ve done just that for this blog, and, despite its linguistic informalities, it has come out with a score of 43.8 on the Flesch-Kincaid reading-ease test, which puts it in the category of ‘Difficult to read’! Looks like it’s a matter of doing as we say, not as we do! Though, in our defence, that’s not easy.
- We tried harder and came up with: ‘People need to know what’s involved in being in a research project. They need to know before they agree to take part. Researchers need to be clear and simple when they tell them. They shouldn’t use jargon. They should use easy words and short sentences. They should think about using different ways to tell different types of people’. That got us a score of 85.2 – ‘Easy to read. Conversational English for consumers,’ which isn’t too bad in that it’s got us over the NCBI’s threshold of a reading age of 11-12 years, but that’s still two years older than the average UK adult’s reading age.

 Today’s spotlight is on the Researchers’ Responsibilities
Today’s spotlight is on the Researchers’ Responsibilities











 SPROUT: From Sustainable Research to Sustainable Research Lives
SPROUT: From Sustainable Research to Sustainable Research Lives BRIAN upgrade and new look
BRIAN upgrade and new look Seeing the fruits of your labour in Bangladesh
Seeing the fruits of your labour in Bangladesh Exploring Embodied Research: Body Map Storytelling Workshop & Research Seminar
Exploring Embodied Research: Body Map Storytelling Workshop & Research Seminar Marking a Milestone: The Swash Channel Wreck Book Launch
Marking a Milestone: The Swash Channel Wreck Book Launch ECR Funding Open Call: Research Culture & Community Grant – Application Deadline Friday 12 December
ECR Funding Open Call: Research Culture & Community Grant – Application Deadline Friday 12 December MSCA Postdoctoral Fellowships 2025 Call
MSCA Postdoctoral Fellowships 2025 Call ERC Advanced Grant 2025 Webinar
ERC Advanced Grant 2025 Webinar Update on UKRO services
Update on UKRO services European research project exploring use of ‘virtual twins’ to better manage metabolic associated fatty liver disease
European research project exploring use of ‘virtual twins’ to better manage metabolic associated fatty liver disease