Congratulations to Dr. Karim Khaled on the latest paper from his BU Ph.D. research. This article ‘Ethical Issues and Challenges Regarding the Use of Mental Health Questionnaires in Public Health Nutrition Research‘ [1] was published earlier this month in the international journal Nutrients.
Karim is currently based at Birmingham City University, and the paper is co-authored with his Ph.D. supervisors Dr. Fotini Tsofliou and Prof. Vanora Hundley in BU’s Faculty of Health & Social Sciences.  This paper addresses the potential burden of completing mental health questionnaires on (a) participants and (b) researchers. This examines ethical issues and challenges of using such scales and questionnaires, providing a real-life case study where the Beck’s Depression Inventory-II was used.
This paper addresses the potential burden of completing mental health questionnaires on (a) participants and (b) researchers. This examines ethical issues and challenges of using such scales and questionnaires, providing a real-life case study where the Beck’s Depression Inventory-II was used.
The ethical considerations raised by using mental health questionnaires in epidemiological research include incorrectly identifying participants as depressed or non-depressed; inability to identify participants for referral procedures due to the anonymous nature of some research studies; an increased burden on participants through depression and suicidal questions; and the high expectation of participants towards the researcher.  Preventative measures to reduce these challenges include choosing appropriate cut-off scores for correctly identifying participants; highlighting whether mental health questionnaires used may elicit negative emotional or psychological reactions related to suicide ideation; specifying the criteria for referral to clinical services; detailing the intended referral processes; including approaches where the researcher directly connects participants with a psychological service provider; and including a passive referral method such as contact details for participants to initiate their own referrals to clinical care. The authors offer a guide for researchers aiming to collect data on mental health through questionnaires, and they conclude that ethical challenges should be considered and reviewed at all stages of the research project.
Preventative measures to reduce these challenges include choosing appropriate cut-off scores for correctly identifying participants; highlighting whether mental health questionnaires used may elicit negative emotional or psychological reactions related to suicide ideation; specifying the criteria for referral to clinical services; detailing the intended referral processes; including approaches where the researcher directly connects participants with a psychological service provider; and including a passive referral method such as contact details for participants to initiate their own referrals to clinical care. The authors offer a guide for researchers aiming to collect data on mental health through questionnaires, and they conclude that ethical challenges should be considered and reviewed at all stages of the research project.
Well done!
Prof. Edwin van Teijlingen

Reference:
- Khaled, K., Tsofliou, F., Hundley, V. (2025). Ethical Issues and Challenges Regarding the Use of Mental Health Questionnaires in Public Health Nutrition Research Nutrients 17 (4): 715. https://doi.org/10.3390/nu17040715

 All research undertaken by BU staff and students is subject to appropriate ethical reflection, leading to a formal ethics review as appropriate.
All research undertaken by BU staff and students is subject to appropriate ethical reflection, leading to a formal ethics review as appropriate.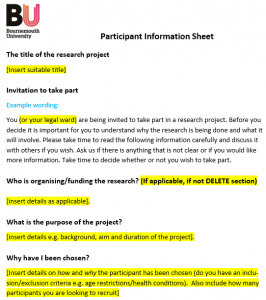












 REF Code of Practice consultation is open!
REF Code of Practice consultation is open! BU Leads AI-Driven Work Package in EU Horizon SUSHEAS Project
BU Leads AI-Driven Work Package in EU Horizon SUSHEAS Project Evidence Synthesis Centre open at Kathmandu University
Evidence Synthesis Centre open at Kathmandu University Expand Your Impact: Collaboration and Networking Workshops for Researchers
Expand Your Impact: Collaboration and Networking Workshops for Researchers ECR Funding Open Call: Research Culture & Community Grant – Apply now
ECR Funding Open Call: Research Culture & Community Grant – Apply now ECR Funding Open Call: Research Culture & Community Grant – Application Deadline Friday 12 December
ECR Funding Open Call: Research Culture & Community Grant – Application Deadline Friday 12 December MSCA Postdoctoral Fellowships 2025 Call
MSCA Postdoctoral Fellowships 2025 Call ERC Advanced Grant 2025 Webinar
ERC Advanced Grant 2025 Webinar Update on UKRO services
Update on UKRO services European research project exploring use of ‘virtual twins’ to better manage metabolic associated fatty liver disease
European research project exploring use of ‘virtual twins’ to better manage metabolic associated fatty liver disease