 Late last week my colleague Dr. Pramod Regmi, Senior Lecturer in International Health, returned home from his Erasmus+ exchange to Nepal. He brought home for me a copy of the MMIHS (Manmohan Memorial Institute of Health Sciences) Souvenir 2023, this outliens key events at the institution of the past year. One of the write ups in the Souvenir is from the seven MMIHS M.Sc. students in Public Health who visited Bournemouth University in late 2022-early 2023 for three months.
Late last week my colleague Dr. Pramod Regmi, Senior Lecturer in International Health, returned home from his Erasmus+ exchange to Nepal. He brought home for me a copy of the MMIHS (Manmohan Memorial Institute of Health Sciences) Souvenir 2023, this outliens key events at the institution of the past year. One of the write ups in the Souvenir is from the seven MMIHS M.Sc. students in Public Health who visited Bournemouth University in late 2022-early 2023 for three months. 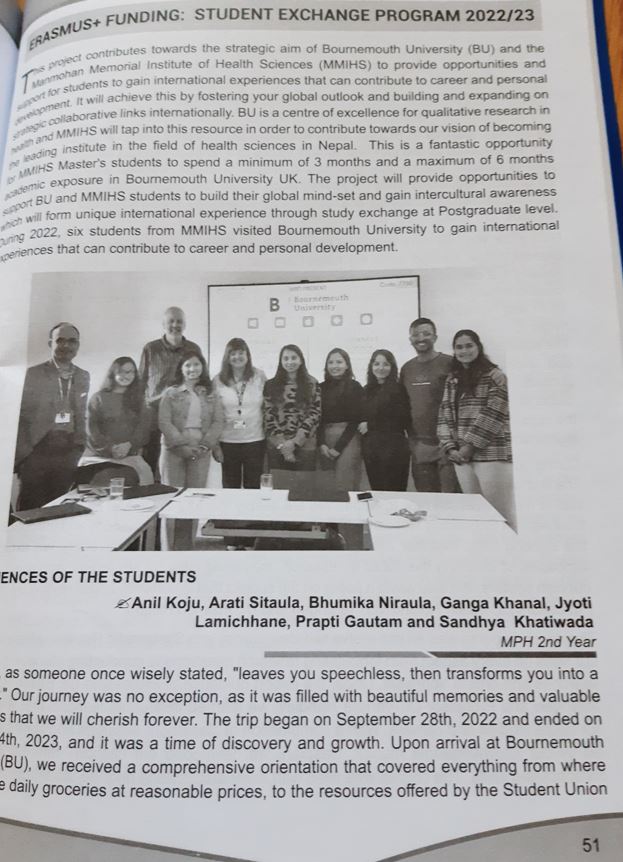 The students have since all completed their M.Sc. in Public Health at MMIHS. Their story highlights some of the British features of student life which were new to them. These included the support they received from our SUBU (=students’ union), or registering with the NHS, and the UNIBUS app, as well as cultural celebrations during their time in Dorset, such Halloween, Christmas and New Year. They rave about the module Public Involvement in Research and specifically thank Dr. Mel Hughes and BU’s PIER (Public Involvement in Education & Research) team. Their second module at BU focused on Systematic Reviewing, they particularly mention the guidance and support received from Prof. Vanora Hundley in the Centre for Midwifery & Women’s Health (CMWH) and our Faculty of Health & Social Sciences librarian Mr. Caspian Dugdale.
The students have since all completed their M.Sc. in Public Health at MMIHS. Their story highlights some of the British features of student life which were new to them. These included the support they received from our SUBU (=students’ union), or registering with the NHS, and the UNIBUS app, as well as cultural celebrations during their time in Dorset, such Halloween, Christmas and New Year. They rave about the module Public Involvement in Research and specifically thank Dr. Mel Hughes and BU’s PIER (Public Involvement in Education & Research) team. Their second module at BU focused on Systematic Reviewing, they particularly mention the guidance and support received from Prof. Vanora Hundley in the Centre for Midwifery & Women’s Health (CMWH) and our Faculty of Health & Social Sciences librarian Mr. Caspian Dugdale.
Unfortunately, the Erasmus+ scheme has come to an end, but Bournemouth University has just been awarded funding for a serious number of Turing Scheme exchanges. The latter is for BU students to go aboard, and this funding supports study exchanges, work placements, voluntary traineeships and other international extra-curricular or curricular activities worldwide for a minimum of 28 days and maximum of 12 months.

Prof. Edwin van Teijlingen
CMWH














 Dr. Ashraf cited on ‘Modest Fashion’ in The Guardian
Dr. Ashraf cited on ‘Modest Fashion’ in The Guardian NIHR-funded research launches website
NIHR-funded research launches website Academics write for newspaper in Nepal
Academics write for newspaper in Nepal New paper published on disability in women & girls
New paper published on disability in women & girls Global Consortium for Public Health Research 2025
Global Consortium for Public Health Research 2025 MSCA Postdoctoral Fellowships 2025 Call
MSCA Postdoctoral Fellowships 2025 Call ERC Advanced Grant 2025 Webinar
ERC Advanced Grant 2025 Webinar Horizon Europe Work Programme 2025 Published
Horizon Europe Work Programme 2025 Published Horizon Europe 2025 Work Programme pre-Published
Horizon Europe 2025 Work Programme pre-Published Update on UKRO services
Update on UKRO services European research project exploring use of ‘virtual twins’ to better manage metabolic associated fatty liver disease
European research project exploring use of ‘virtual twins’ to better manage metabolic associated fatty liver disease