Women Academics Centre Stage in Presidential Roles in Major International Professional Bodies and Conference Organisation
3rd International Sociological Association Forum of Sociology
10-14 July2016, University of Vienna, Austria
Professor Ann Brooks
Bournemouth University
This year’s Third ISA was held at the University of Vienna and shortly after Brexit, so I braced myself to face a barrage of jokes and recriminations about the UK vote. Well there was some gentle humour in the plenaries but the response was mainly one of pity. The conference was based in the opulence of the University of Vienna… . With its historical and contemporary position in relation to both European and global sociology this conference attracted 4,000 sociologists from across the globe. I usually find the ISA a somewhat unwieldy conference compared to the BSA and ASA but Research Committtee (RC) 32 Women in Society, has a wonderfully inclusive feel and gave coherence to the entire conference for me (see below). Increasingly some of the best conferences have women centre stage, including the ASA 2015 Conference in Chicago, with the then ASA President, Paula England, and the current ASA President and Chair of the 2016 Program Committee, Ruth Milkman (CUNY –Graduate Centre). The ASA Conference was held in Seattle in August 2016. The current ISA President is Margaret Abraham (Hofstra University, USA) who together with a team at the University of Vienna delivered a conference which did not disappoint.

A series of important and thoughtful plenaries addressed the global dimensions of the conference with the University of Vienna organising team providing an interesting European dimension addressing the Brexit issue. A generally favourable balance was achieved between global and European dimensions. The Opening Plenary featured a number of academics from the University of Vienna and they were clearly delighted at attracting over 5,000 sociologists to this impressive university as the conference base. The Dean of the Faculty of Social Sciences at the University of Vienna, Ulrike Felt, provided an uplifting and impressive summary of the social sciences at the University Vienna and I can see the number of applicants for positions there escalating as a result. It was also great to see governmental support for the social sciences, with Barbara Weitgruber, Director General, Austrian Ministry of Science delivering a very positive statement in support of the social sciences. Margaret Abraham’s ISA Presidential Address, found here:
http://www.isa-sociology.org/forum-2016/
https://www.youtube.com/watch?v=LW44_sW4Jmc
was an important statement in equity and intersectionality and made an important contribution to this lively opening Plenary. Margaret is also an important contributor to the ASA Conference, particularly in terms of the International aspects of both conferences.
While the conference lacked the celebrity appeal of the ASA, it certainly did not lack in the seriousness of the debates. One of the most interesting debates came from the closing plenary chaired by Marcus Schultz (New School for Social Research, New York), with Asef Bayat (University of Illinois) ‘Imagining a Post-Islamist Democracy’, Akosua Adomako Ampofo (University of Ghana) ‘Black Lives Matter and the Status of the African World’, Todd Gatlin (Columbia) ‘What Kind of a World Can Weather Climate Change?’ and Alain Touraine (Ecole des Hautes Etudes en Science Sociales, France), as discussant.
Research Committee (RC) 32 Women in Society
The size of the conference meant that affiliation to specific programs proved a favoured response. I am a member of RC32 Women in Society and the program was widely regarded as one of the best at the conference. The Program Coordinators for RC32, Akosua Adomako Ampofo and Josephine Beoku-Betts (Florida Atlantic) had worked to organise an extensive range of panels and roundtables including: ‘Human Trafficking: The Labour and Sexual Exploitation of Women and Children’; ‘Twenty Years after Beijing: A Cross-National Approach to Feminist Movements and the Implementation of the Platform for Action’; ‘Global Sociology and Feminist Perspectives on Care, Care Work and the Struggle for a Careful World’; ‘Knowledge Production: Feminist Perspectives in the 21st Century’; ‘Gender, Law and the Courts: Local and Global Struggles Against Violence’; ‘ Intersectionalities of Power in Research: Strategies for Action and Justice’; ‘Gender, Culture and Technologies in the Knowledge Economy’; ‘Muslim Women’s Struggles for a Better World through Promoting Gender Equality’; and ‘The Cities We Want: Using Visionary Methodologies to Create Feminist Alternatives to Urban Planning’. My paper was in the ‘Precarity and Gender in the Era of Neoliberal Globalization’ and I focused on relational precarity as highlighted in the work of Lauren Berlant entitled: ‘Gender, Precarity and Sexuality: The Intersection of Gender, Ethnicity, Sexuality and Class in Relational Precarity in Neoliberal Society–the Influence of Lauren Berlant’. .
The double badging of sessions with RC32 with other RCs was a really valuable dimension of the conference, this was particularly the case for the RC02 Economy and Society led by the Program Coordinator, Heidi Gottfried, which included some excellent sessions including: ‘Gender Regimes or Gendered Institutions’ organised by Sylvia Walby. A particularly interesting session was the ‘Author Meets Critics: Crisis by Sylvia Walby’. Chaired by Heidi Gottfried and with discussants Stephanie Woehl (Vienna) and Christopher Chase-Dunn (California-Riverside). This proved to be one of the most coherent and intense social and political analyses including the focus on the EU and had anticipated Brexit. Sylvia’s response to criticism was powerful and wide-ranging and pointed to the next political crisis being in the EU not the UK. She also calls for a ‘regendering of the political project’.

This was a really fascinating conference, serious in its debates and commemorating the work and loss of John Urry.
Professor Ann Brooks
August 2016
 COST (European Cooperation in Science and Technology) is a unique platform where European researchers can jointly develop their ideas and initiatives across all scientific disciplines through trans-European networking of nationally funded research. Preeti pal has been awarded the sum of 500 euro to cover the cost of attending the Training School and travel and accommodation costs. Preeti’s PhD project is on maternity care provision in Nepal. Preeti’s research focuses on the quality and equity of service available at birthing centres. In Nepal, birthing centres act as first contact point for the women seeking maternity services especially the basic obstetric care. She is supervised by Dr. Catherine Angell, Prof. Edwin van Teijlingen and BU Visiting Faculty Prof. Padam Simkhada (based at Liverpool John Moores University).
COST (European Cooperation in Science and Technology) is a unique platform where European researchers can jointly develop their ideas and initiatives across all scientific disciplines through trans-European networking of nationally funded research. Preeti pal has been awarded the sum of 500 euro to cover the cost of attending the Training School and travel and accommodation costs. Preeti’s PhD project is on maternity care provision in Nepal. Preeti’s research focuses on the quality and equity of service available at birthing centres. In Nepal, birthing centres act as first contact point for the women seeking maternity services especially the basic obstetric care. She is supervised by Dr. Catherine Angell, Prof. Edwin van Teijlingen and BU Visiting Faculty Prof. Padam Simkhada (based at Liverpool John Moores University).













 Public Health England has launched a
Public Health England has launched a 



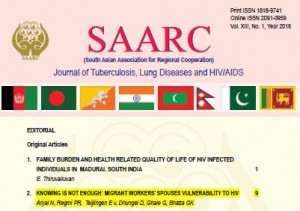



 Congratulations to Dr. Pramod Regmi as the lead author of the paper ‘
Congratulations to Dr. Pramod Regmi as the lead author of the paper ‘


















 No access to BRIAN 5-6th February
No access to BRIAN 5-6th February Missing Persons Indicator Project Recruitment
Missing Persons Indicator Project Recruitment Celebrating our Research: Postgraduate Research Showcase 2026
Celebrating our Research: Postgraduate Research Showcase 2026 Nursing Research REF Impact in Nepal
Nursing Research REF Impact in Nepal Fourth INRC Symposium: From Clinical Applications to Neuro-Inspired Computation
Fourth INRC Symposium: From Clinical Applications to Neuro-Inspired Computation ESRC Festival of Social Science 2025 – Reflecting back and looking ahead to 2026
ESRC Festival of Social Science 2025 – Reflecting back and looking ahead to 2026 ECR Funding Open Call: Research Culture & Community Grant – Apply now
ECR Funding Open Call: Research Culture & Community Grant – Apply now MSCA Postdoctoral Fellowships 2025 Call
MSCA Postdoctoral Fellowships 2025 Call ERC Advanced Grant 2025 Webinar
ERC Advanced Grant 2025 Webinar Update on UKRO services
Update on UKRO services European research project exploring use of ‘virtual twins’ to better manage metabolic associated fatty liver disease
European research project exploring use of ‘virtual twins’ to better manage metabolic associated fatty liver disease