TEF
Wonkhe bloggers imagine alternative ways to run (ideally improve) the TEF in Visions for the AlterniTEF – can we do TEF better? Ideas ranged from:
- individual institution-specific targets as a condition of registration OfS (and therefore accountable under the Higher Education and Research Act);
- metrics produced through relational analyses and cross referencing – this complex idea stemmed from measuring the quality and impact of reciprocal relationships;
- individual learning statements setting institutional goals which the provider would be measured against – similar to current Fair Access Agreement;
- ignoring undergraduate TEF and focusing on bringing post-graduate TEF online, including the influence of social capital and the added value of the post-graduate qualification on social mobility. This approach controversially espouses a metrics only approach and abolishes the provider statements.
Wonkhe also continue to unpick the influence of the provider statement in changing an institution’s initial metrics-based TEF rating. Marking the TEF creative writing challenge suggests the panel compensated providers who appeared to be effectively addressing poor NSS scores, took into account a London effect, and rewarded institutions with successful outcomes for part time study.
Brexit and Erasmus
A Times Higher article on the alternative to Erasmus post-Brexit highlights the downsides inherent in an Erasmus alternative. The EU exit agreement will determine whether the UK continues to participate in Erasmus, however, the government is currently pursuing a hard line on free movement which decreases the likelihood Erasmus would continue in its current form. An alternative is to establish bilateral agreements to exchange students with key European universities – just as we do now with international institutions. However, the article highlights the negative impact on social mobility – bilateral agreements mean the students must cover their own costs to some extent – decreasing the likelihood lower income students could afford to participate. While the obvious answer (to divert the UK’s contribution to the EU budget which funds Erasmus to a home-grown scheme) seems reasonable the budget required would be in excess of €113 million and the government have yet to confirm this as an option. Furthermore the time and administrative costs for universities to individually negotiate grants and agreements is excessive. The article also touches on lower demand from EU students to come to the UK suggesting exchanges may not be viable.
Parliamentary Questions
Q: Catherine West: What discussions he has had with the Secretary of State for Education on the future of the UK’s participation in the Erasmus scheme.
A: Mr Steve Baker: The Department has regular conversations with officials and Ministers from other governmental departments about a range of policy issues arising from EU exit. With regards to the Erasmus+ programme, the Government recognises the value of international exchange and collaboration in education as part of our vision for the UK as a global nation. There may be European programmes in which we wish to continue to participate after we exit. This will be considered as part of ongoing negotiations with the European Union
Brexit – staff and students
The Russell Group published 10 points requiring greater clarity in response to the UK Government’s position on EU nationals. This included calling for:
- ensuring academic and student time abroad for study, training, career development and research purposes does not negatively impact on continuous residency
- interpreting ‘strong ties’ broadly to ensure academics and students spending 2+ years abroad do not lose their settled status once this has been established
- EU students starting courses in 2017/18 and 2018/19 should be able to stay and work here after their studies and be eligible for settled status after accruing five years residence
- ensuring that professional qualifications obtained in either the UK or the EU before the UK’s withdrawal continue to be recognised across borders
Education-related exports and transnational education activity
The government released experimental statistics estimating the value of exports from the UK education section, the respective contribution of the higher and further education sectors, and transnational activity for 2010-2014. (Transnational education is education provided in a country different to that of the awarding institution.) The total value was estimated to be £18.76 billion – an increase of 18% against 2010. HE was the main contributor accounting for 92% of the total value, with revenue from transnational education contributing the remaining 8%. The full report is here.
Accompanying the experimental statistics is a report analysing the value of transnational education to the UK (originally published November 2014). The report discusses the benefits of transnational education to UK HE institutions (see page 11 for a summary).
Nursing & midwifery places
The Royal College of Nursing spoke out this week highlighting the discrepancy between the Government’s plans to expand the mental health workforce and the significant downturn in nursing applications attributed to the introduction of fees and the withdrawal of the NHS bursary. The Government has earmarked £1.3 billion for mental health services, pledging to treat an additional one million patients by 2020-21 through 24/7 services. The RCN says there is already a dangerous lack of workforce planning and accountability, and warns the Government will need to work hard just to get back to the number of specialist staff working in mental health services in 2010. They state that under this Government there are 5,000 fewer mental health nurses.
Janet Davies, RCN Chief Executive & General Secretary, expressed skepticism at the government’s plans and stated: “If these nurses were going to be ready in time, they would be starting training next month…but we have seen that the withdrawal of the bursary has led to a sharp fall in university applications and we are yet to see funding for additional places.” [The government previously stated the removal of bursaries will mean an additional 10,000 training places for healthcare students could be made available by 2020.]
On the ending of the bursary Jon Skewes, Director, at Royal College of Midwives (RCM) said: ‘We believe this decision is a fundamental mistake by the government and have warned about the wide reaching implications of removing the student midwifery bursary given the existing crisis in our maternity services. In England alone we remain 3500 midwives short. This, coupled with younger midwives leaving, an ageing workforce and the loss of EU midwives post-Brexit, means the RCM has grave concerns for staffing our maternity services. The government has completely ignored RCM advice to make any loans forgivable if students then go to work in the NHS. The axing of the bursary and introduction of tuition in England will without doubt worsen the current shortage of midwives.’
Tuition Fees
The Centre for Policy Studies released an Economic Bulletin on tuition fees: Wealthy Graduates: The Winners from Corbyn’s tuition fees plan. It reiterates known messages including increases in disadvantaged pupils accessing HE and the social unfairness of expecting non-graduates to subsidise education for degree students. It also makes the following points:
- The maximum fee ceiling is charged by most universities, there is little differentiation. This means the intended competitiveness was unsuccessful as there is no clear link between tuition fees paid and job prospects. (See page 8 of the full report for more detail.) While TEF still intends to differentiate fees paid on quality the scale of the difference is limited.
- It calls on ministers to avoid retrospectively increasing graduate’s fee repayments, to consider reducing loan interest rates, and to incentivise courses linking to labour shortages.
- It also recommends policy makers consider intergenerational fairness but without abolishing tuition fees
- Scotland’s previous no tuition fee policy which resulted in a student numbers cap means their social mobility outcomes are lower than England’s.
Widening Participation
Statistics – progression and outcome
The Department for Education have published statistics on the 2014/15 entry cohort – Widening Participation in HE. These are the regular annual statistics detailing young participation in HE with social background comparisons and graduate outcomes. Headlines:
- The progression rate of free school meals (FSM) pupils has increased, but so has the gap between FSM and non-FSM. Page 5 has a diagram breaking this down by region.
- The state school Vs independent school gap in progressing to the most selective HE institutions has widened slightly
- Graduate outcomes – disadvantaged students employed in the most advantaged occupations is up by 1%, although the gap between most and least advantaged students in these high-end jobs remains static at 6%.
School-age attainment trends
The Education Policy Institute has published Closing the Gap? Trends in Educational Attainment and Disadvantage. The report focuses on school aged children analysing the attainment gaps between children from disadvantaged backgrounds and their peers plus other pupil characteristics. It covers the progress made, the enduring challenges (including magnitude of learning gaps and lack of progress for the most persistently disadvantaged pupils). It recommends an additional 8 local authority districts on top of the 12 Opportunity Areas currently identified by the Department for Education. Finally, it states that without significant acceleration in the rate at which gaps are being addressed it take until 2070 before disadvantaged children did not fall further behind other students during their time in education.
UK UG Vs International Student numbers
The Sunday Times led with an article claiming universities recruitment of the financially more lucrative international students was crowding out intake of UK undergraduates: Universities take foreign students ahead of British.
The sector responded on Twitter and Wonkhe set out what is misleading in the Times article in their blog: What the Sunday Times got Wrong. This states that the Times article used inappropriate statistics and reminded that UK school leavers now enter university at the highest ever levels.
David Morris (Wonkhe) writes: when I confronted Gilligan about this on Twitter, his response suggested (to me at least) a realisation that a mistake had been made. He argued that his piece “was mainly about the fact that non-EU undergrads are admitted with lesser qualifications” and that we shouldn’t suggest that part-time and second degree students “don’t count”.
In his critique Morris also acknowledges the difficulty navigating HESA statistics for the uninitiated: HESA’s website is not the easiest to use, and one could easily look at overall undergraduate numbers and make an assumption about a story that simply isn’t there. I would urge HESA to make finding historic data more ‘journalist friendly’ for hacks with a deadline. To write this piece I have had to have six different tabs open on HESA’s website, plus three different Excel sheets and the HESA mobile app. No wonder mistakes can be made.
Case Studies
Universities UK have published a directory of case studies illustrating how universities are tackling harassment, violence against women and hate crime. The case studies cover a range of areas including prevention, improving incident reporting procedures, effective responses, student and staff training, and good practice.
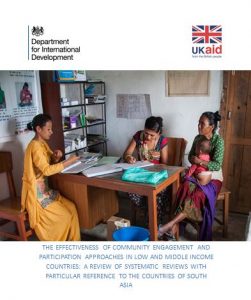
 This weekend Manmohan Memorial Institute of Health Sciences (MMIHS) in Kathmandu, Nepal signed a Memorandum of Agreement (MoA) with Bournemouth University (BU).
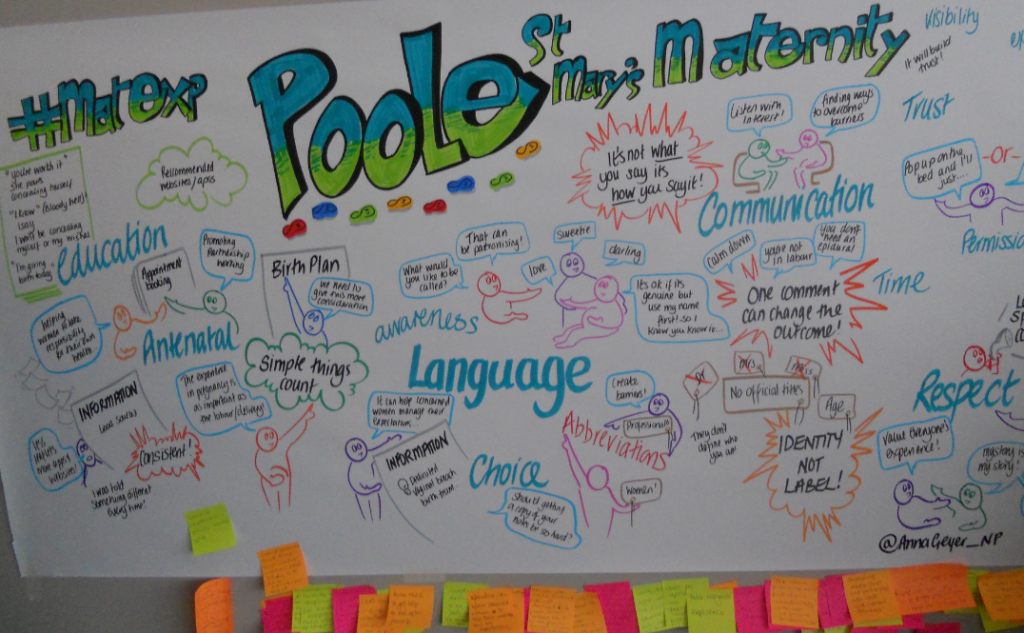
This weekend Manmohan Memorial Institute of Health Sciences (MMIHS) in Kathmandu, Nepal signed a Memorandum of Agreement (MoA) with Bournemouth University (BU).  The ceremonial signing took place on the final day (24th Feb.) of the International Conference on Quality Education in Federal Nepal. Prof. Stephen Tee, who also spoke at the conference, represented our university.
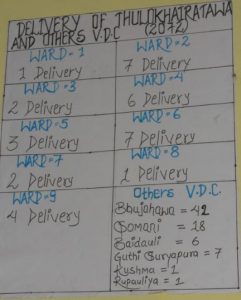
The ceremonial signing took place on the final day (24th Feb.) of the International Conference on Quality Education in Federal Nepal. Prof. Stephen Tee, who also spoke at the conference, represented our university. The UoA formalises a long-standing collaboration between the two institutions. MMIHS and BU academics have jointly applied for research grants, conducted collaborative research and published together. Several BU staff [1-3] and students [4] in the Faculty of Health & Social Sciences have published in the Journal of Manmohan Memorial Institute of Health Sciences, an Open Access journal. Moreover, Prof. Edwin van Teijlingen in the Centre for Midwifery, Maternal and Perinatal Health has been a Visiting Professor at MMIHS for nearly a decade and has given several guest lectures over the years to staff and students at MMIHS.
The UoA formalises a long-standing collaboration between the two institutions. MMIHS and BU academics have jointly applied for research grants, conducted collaborative research and published together. Several BU staff [1-3] and students [4] in the Faculty of Health & Social Sciences have published in the Journal of Manmohan Memorial Institute of Health Sciences, an Open Access journal. Moreover, Prof. Edwin van Teijlingen in the Centre for Midwifery, Maternal and Perinatal Health has been a Visiting Professor at MMIHS for nearly a decade and has given several guest lectures over the years to staff and students at MMIHS.











 Our
Our 













 Dr. Ashraf cited on ‘Modest Fashion’ in The Guardian
Dr. Ashraf cited on ‘Modest Fashion’ in The Guardian NIHR-funded research launches website
NIHR-funded research launches website Academics write for newspaper in Nepal
Academics write for newspaper in Nepal New paper published on disability in women & girls
New paper published on disability in women & girls Global Consortium for Public Health Research 2025
Global Consortium for Public Health Research 2025 MSCA Postdoctoral Fellowships 2025 Call
MSCA Postdoctoral Fellowships 2025 Call ERC Advanced Grant 2025 Webinar
ERC Advanced Grant 2025 Webinar Horizon Europe Work Programme 2025 Published
Horizon Europe Work Programme 2025 Published Horizon Europe 2025 Work Programme pre-Published
Horizon Europe 2025 Work Programme pre-Published Update on UKRO services
Update on UKRO services European research project exploring use of ‘virtual twins’ to better manage metabolic associated fatty liver disease
European research project exploring use of ‘virtual twins’ to better manage metabolic associated fatty liver disease