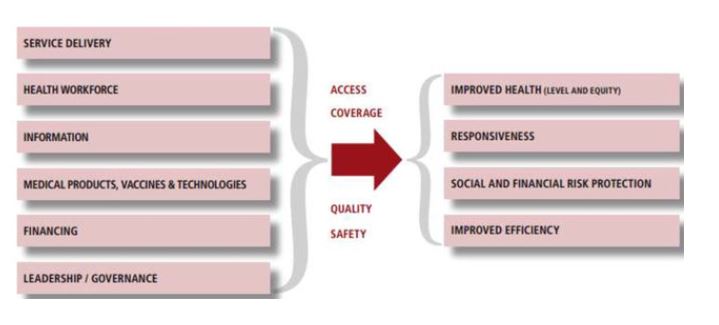
This week the Nepal Federal Health System Team published its latest paper the international journal Health Research Policy & Systems [1]. This Open Access paper ‘Overcoming the challenges facing Nepal’s health system during federalisation: an analysis of health system building blocks‘ reports on two separate methods: interviews and participatory policy analysis workshops, to offer an in-depth understanding of stakeholders’ practical learning, experiences, and opinions. Participants included policymakers, health service providers, local elected members, and other local stakeholders. All interviews were audio-recorded, transcribed, translated into English, and analysed thematically using the six WHO (World Health Organization) health system building blocks [2] as its theoretical framework. 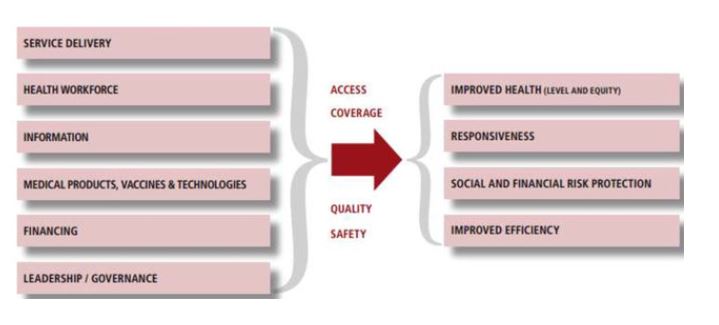
Wasti et al. found that participants noted both opportunities and challenges around each building block. Identified opportunities were: (a) tailored local health policies and plans, (b) improved health governance at the municipality level, (c) improved health infrastructure and service capacity, (d) improved outreach services, (e) increased resources (health budgets, staffing, and supplies), and (f) improved real-time data reporting from health facilities. At the same time, several challenges were identified including: (a) poor coordination between the tiers of government, (b) delayed release of funds, (c) maldistribution of staff, (d) problems over procurement, and (e) limited monitoring and supervision of the quality of service delivery and data reporting.
The paper concludes that since federalisation, Nepal’s health system performance is improving, although much remains to be accomplished. For Nepal to succeed in its federalisation process, understanding the challenges and opportunities is vital to improving each level of the health system in terms of (a) leadership and governance, (b) service delivery, (c) health financing, (d) health workforce, (e) access to essential medicines and technologies and (f) health information system.
This publication is the fourth one originating from our Nepal Federal Health System Project, our major collaborative project examining the consequences for the health system of Nepal’s move to a federal government structure [2-5]. This is a joint project (2020-2024) led by the University of Sheffield and in collaboration with Bournemouth University, the University of Huddersfield, Manmohan Memorial Institute of Health Sciences (MMIHS) and PHASE Nepal. This longitudinal interdisciplinary study is funded by the UK Health Systems Research Initiative [Grant ref. MR/T023554/1].
Prof. Edwin van Teijlingen
Centre for Midwifery & Women’s Health (CMWH)
References:
- Wasti, S.P., van Teijlingen, E.,Rushton, S., Subedi, M., Simkhada, P., Balen, J. for the Nepal Federal Health System Team (2023) Overcoming the Challenges Facing Nepal’s Health System During Federalisation: An Analysis of Health System Building Blocks, Health Research Policy & Systems 21(117) https://doi.org/10.1186/s12961-023-01033-2
- World Health Organization (2007) Everybody’s business: strengthening health systems to improve health outcomes. WHO’s Framework for Action. Geneva: World Health Organization.
- Sapkota, S., Panday, S., Wasti, S.P., Lee, A., Balen, J., van Teijlingen, E., Rushton, S., Subedi, M., Gautam, S., Karki., J., Adhikary, P., Marahatta, S., Simkhada, P., for the Nepal Federal Health System Team (2022) Health System Strengthening: The Role of Public Health in Federal Nepal, Journal of the Nepal Public Health Association 7(1):36-42.
- Adhikary, P., Balen, J., Gautam, S., Ghimire, S., Karki, J., Lee, A.C.K., Marahatta, S.B., Panday, S., Pohl, G., Rushton, S., Sapkota, S., Simkhada, P.P., Subedi, M., van Teijlingen, E. for the Nepal Federal Health System team (2020) The COVID-19 pandemic in Nepal: Emerging evidence on the effectiveness of action by, and cooperation between, different levels of government in a federal system, Journal of Karnali Academy of Health Sciences 3 (3): 1-11.
- Rushton, S., Pandey, S., van Teijlingen, E., Subedi, M., Balen, J., Karki, J., Simkhada, P. on behalf of the Nepal Federal Health System Team (2021) An Investigation into the Impact of Decentralization on the Health System of Nepal. Journal of Manmohan Memorial Institute of Health Sciences, 7(1): 3–14. https://doi.org/10.3126/jmmihs.v7i1.43146
 Early next week Prof. Edwin van Teijlingen from the Centre for Midwifery & Women’s Health (CMWH) has been invited to present online at the International Evidence Synthesis Workshop on November 13th in Qatar. His presentation will focus on key aspects of writing up systematic reviews. The workshop is organised by the WHO (World Health Organization) Collaborating Centre for Healthy Ageing and Dementia.
Early next week Prof. Edwin van Teijlingen from the Centre for Midwifery & Women’s Health (CMWH) has been invited to present online at the International Evidence Synthesis Workshop on November 13th in Qatar. His presentation will focus on key aspects of writing up systematic reviews. The workshop is organised by the WHO (World Health Organization) Collaborating Centre for Healthy Ageing and Dementia. 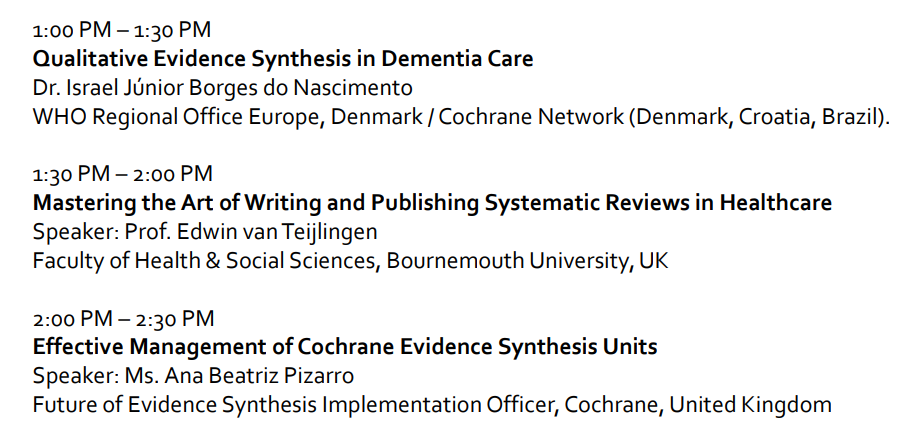


















 REF Code of Practice consultation is open!
REF Code of Practice consultation is open! BU Leads AI-Driven Work Package in EU Horizon SUSHEAS Project
BU Leads AI-Driven Work Package in EU Horizon SUSHEAS Project Evidence Synthesis Centre open at Kathmandu University
Evidence Synthesis Centre open at Kathmandu University Expand Your Impact: Collaboration and Networking Workshops for Researchers
Expand Your Impact: Collaboration and Networking Workshops for Researchers Visiting Prof. Sujan Marahatta presenting at BU
Visiting Prof. Sujan Marahatta presenting at BU ECR Funding Open Call: Research Culture & Community Grant – Apply now
ECR Funding Open Call: Research Culture & Community Grant – Apply now ECR Funding Open Call: Research Culture & Community Grant – Application Deadline Friday 12 December
ECR Funding Open Call: Research Culture & Community Grant – Application Deadline Friday 12 December MSCA Postdoctoral Fellowships 2025 Call
MSCA Postdoctoral Fellowships 2025 Call ERC Advanced Grant 2025 Webinar
ERC Advanced Grant 2025 Webinar Update on UKRO services
Update on UKRO services European research project exploring use of ‘virtual twins’ to better manage metabolic associated fatty liver disease
European research project exploring use of ‘virtual twins’ to better manage metabolic associated fatty liver disease