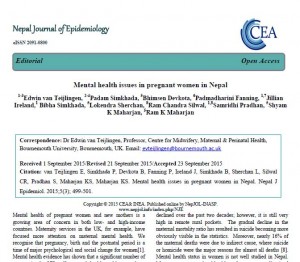
FHSS PhD student Rachel Arnold has been quoted in of one world’s most famous newspapers The New York Times. Late last week on Dec. 4th The New York Times published an article under the heading ‘Reported Gains in Afghan Maternal Health Are Found to Be Implausible’ [1]. Rachel Arnold was interviewed since her PhD study, based in CMMPH, focuses on maternity care in one of the larger hospitals in the Afghan capital Kabul. Rachel has also published an excellent paper from her research in Afghanistan in the scientific journal BJOG [2]. Her paper analyses the culture of a Kabul maternity hospital to understand its impact on the care of perinatal women and their babies. The paper is published in Gold Open Access, hence freely available to audiences across the globe,
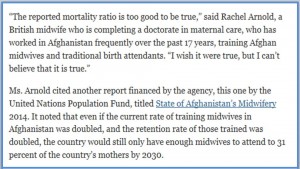
Congratulations.
Prof. Edwin van Teijlingen
Centre for Midwifery, Maternal & Perinatal Health
References:
- Nordland. R. ‘Reported Gains in Afghan Maternal Health Are Found to Be Implausible’ The New York Times Dec 4th, 2015, see: http://www.nytimes.com/2015/12/05/world/asia/afghanistan-maternal-mortality-rate.html
- Arnold R, van Teijlingen E, Ryan K, Holloway I. Understanding Afghan health care providers; a qualitative study of the culture of care in a Kabul maternity hospital. BJOG 2015: 122(2): 260–267.


























 BU attendance at third annual GCPHR meeting in June
BU attendance at third annual GCPHR meeting in June Interactive Tangible and Intangible Heritage Applications – BU student work featured in new book chapter
Interactive Tangible and Intangible Heritage Applications – BU student work featured in new book chapter Second NIHR MIHERC meeting in Bournemouth this week
Second NIHR MIHERC meeting in Bournemouth this week MSCA Postdoctoral Fellowships 2025 Call
MSCA Postdoctoral Fellowships 2025 Call ERC Advanced Grant 2025 Webinar
ERC Advanced Grant 2025 Webinar Horizon Europe Work Programme 2025 Published
Horizon Europe Work Programme 2025 Published Horizon Europe 2025 Work Programme pre-Published
Horizon Europe 2025 Work Programme pre-Published Update on UKRO services
Update on UKRO services European research project exploring use of ‘virtual twins’ to better manage metabolic associated fatty liver disease
European research project exploring use of ‘virtual twins’ to better manage metabolic associated fatty liver disease