A lovely day by the river Stour on Friday 24th saw around 40 delegates and Bournemouth University staff come together to celebrate the launch of the National Centre for Post Qualifying Social Work’s new Mental Capacity Toolkit- mentalcapacitytoolkit.co.uk.
Funded by the Burdett Trust for Nursing, the toolkit aims to provide easily accessible learning materials and information for nurses and other professionals and is a web-based tool which can be accessed wherever a professional has access to the internet.
The project team, led by Professor Lee-Ann Fenge, Director of the NCPQSW and the Centre for Seldom Heard Voices and Principal Investigator Dr Sally Lee, undertook an 18-month long research project investigating the issues that professionals encounter in using the Mental Capacity Act 2005 and what could help to increase knowledge and understanding of the legislation and practice requirements.
The day started with an introduction into the NCPQSW and Centre for Seldom Heard Voices wider work and resources by Professor Fenge before Mike Lyne, Programme Lead for the MCA 2005 at BU and a member of the project team took delegates through the context of past and current mental capacity work at BU with a short tour of future developments. Dr Lee and Dr Debbie Slate then introduced delegates to the research themes and the detail of the project.
Dr Mel Hughes, co-director of the Centre for Seldom Heard Voices and Stevie Corbin-Clarke from the project team followed by discussing a project that they have been working on with the charity National Voices, looking at how the introduction of remote service models during the Covid-19 pandemic has affected vulnerable people and those without internet access.
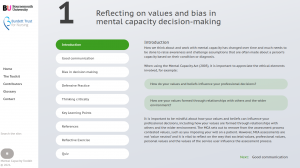
After a light lunch and a warmup quiz, Emily Rosenorn-Lanng introduced the online toolkit and encouraged delegates to log on and have a “play”, and to provide the project team with immediate feedback. Comments included, “I like the visual aspect of the tool” and “I really like the reflective nature of the tool and the questions it asks” and “the quizzes are great!”
Suggestions for further developments were also made with the addition of a search function being a particular desire, which the project team hope to be able to provide this week. Another item on the wish list was the ability to print out a certificate of completion for CPD purposes. The toolkit is very much a work in progress and will be added to over the course of the next few months. The project team are happy to receive feedback and suggestions via the “contact us” details on the NCPQSW website. The toolkit can be accessed at mentalcapacitytoolkit.co.uk.
Here are some example pages of what is included in the tool:

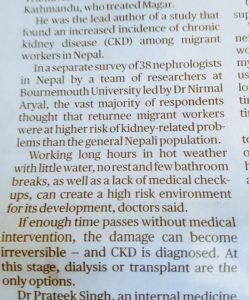
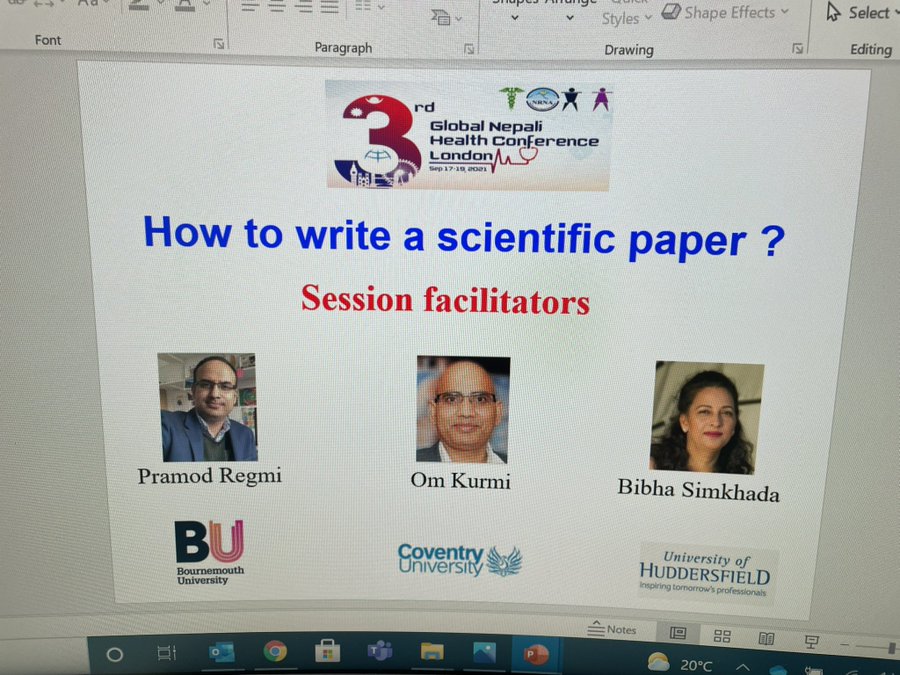
 Dr. Pramod Regmi, Senior Lecturer in International Health in the Department of Nursing Science, has been invited to speak at the forthcoming NIRI Webinar on this Saturday (27th November 2021). He will be jointly presenting with Dr. Nirmal Aryal, Visiting Faculty at the Department of Health & Social Sciences (FHSS). Pramod and Nirmal will be speaking on ‘The hidden health costs of Nepali labour migrants’, following the coverage of Bournemouth University’s research on this topic in The Sunday Times the weekend before last.
Dr. Pramod Regmi, Senior Lecturer in International Health in the Department of Nursing Science, has been invited to speak at the forthcoming NIRI Webinar on this Saturday (27th November 2021). He will be jointly presenting with Dr. Nirmal Aryal, Visiting Faculty at the Department of Health & Social Sciences (FHSS). Pramod and Nirmal will be speaking on ‘The hidden health costs of Nepali labour migrants’, following the coverage of Bournemouth University’s research on this topic in The Sunday Times the weekend before last.































 Beyond Academia: Exploring Career Options for Early Career Researchers – Online Workshop
Beyond Academia: Exploring Career Options for Early Career Researchers – Online Workshop UKCGE Recognised Research Supervision Programme: Deadline Approaching
UKCGE Recognised Research Supervision Programme: Deadline Approaching SPROUT: From Sustainable Research to Sustainable Research Lives
SPROUT: From Sustainable Research to Sustainable Research Lives BRIAN upgrade and new look
BRIAN upgrade and new look Seeing the fruits of your labour in Bangladesh
Seeing the fruits of your labour in Bangladesh ECR Funding Open Call: Research Culture & Community Grant – Apply now
ECR Funding Open Call: Research Culture & Community Grant – Apply now ECR Funding Open Call: Research Culture & Community Grant – Application Deadline Friday 12 December
ECR Funding Open Call: Research Culture & Community Grant – Application Deadline Friday 12 December MSCA Postdoctoral Fellowships 2025 Call
MSCA Postdoctoral Fellowships 2025 Call ERC Advanced Grant 2025 Webinar
ERC Advanced Grant 2025 Webinar Update on UKRO services
Update on UKRO services European research project exploring use of ‘virtual twins’ to better manage metabolic associated fatty liver disease
European research project exploring use of ‘virtual twins’ to better manage metabolic associated fatty liver disease