 This year several students have been funded to work as student research assistants on Fusion Funded-projects.
This year several students have been funded to work as student research assistants on Fusion Funded-projects.
Here, BU MSc student Renuka Balasundaram reflects on her experience of taking part in the scheme and completing the project.
Then, her supervisors Dr Samuel Nyman and Louise Fazakarley share their experiences and encourage staff to participate in the next scheme.
MSc Student reflection
“My experience as a research assistant on the NHS Quality Improvement Project 2017”
Renuka Balasundaram
Department of Psychology
Bournemouth University
My voyage to explore the depths into the field of psychology started when I set off for my Masters in Neuropsychology in Bournemouth University right after my completion of Bachelors in psychology from India. The overwhelming coursework aside, the curriculum of teaching as a whole, felt very different. Three months into my master’s and having adapted myself in totally different environs, I decided to take a leap into the unknown by applying for post of SRA for the fusion funded program project, “NHS Quality Improvement Project”. A week after my successful interview with the project supervisors Dr. Samuel Nyman and Louise Fazakarley, I got a mail about my selection in the project which gave me mixed feelings of exhilaration and apprehension. The mixed emotions were mainly because it was my very first involvement in a practical research project involving hospital setup and interaction with patients. Things gradually settled after my induction with the Christchurch day hospital team and since then it had been a happy workplace with a very helpful and welcoming team at the hospital throughout the project. After a clear briefing of the work to be carried out in the hospital by my supervisors, I made regular visits to the hospital twice a week for almost two months followed by a month of data analysis and report writing. At every step of the project, I got full support from my supervisors which aided in the successful completion of the project. With regards to the project, we aimed to evaluate the Otago exercise training programme in Christchurch day hospital for which I used to regularly interact with the team and patients to get background knowledge and feedback about the training. In spite of having completed research modules in my bachelors and masters, as opposed to theory, it felt completely different when dealing with older patients as participants in a real life setting and collecting data from them through observation and regular interaction.
Personally, this research experience has given me insights into research in a real world and practical setting, enhanced my report writing skills and ultimately putting me firmly in pursuit of my future goal of becoming PhD laureate. It has also given me insight in to the meaning and importance of empirical evidence and scientific backup, for when patients come with a belief and hope of improvement after participation in the study. The project not only had a positive impact on me, but also on the hospital team whereby they implemented many of our suggestions and were pleased with our feedback. As learning and transition is key to growth and development, I strongly feel this project has achieved that, by paving way for an improved quality of training which would ultimately benefit the older population.
Supervisors reflection
We had a Student Research Assistant work with us on a quality improvement project based at Christchurch Day Hospital. Working with the Falls Prevention Team, a student (Renuka) conducted an audit of current practice in the Otago exercise programme with a view to improving patient care. We gained service user feedback, reviewed and analysed the data they had collected, and sought to recommend changes to increase their patients’ exercise practice outside of classes. The project culminated with a report that Renuka presented to the team. Two aspects made this project particularly rewarding:
Learning opportunity for the student
Renuka, a psychology student, had a unique opportunity to work with non-psychology NHS staff as part of a multi-disciplinary team. She was also able to see the importance of research in a real-life context, giving a new depth of understanding to design features. We were also pleased to see our detailed feedback on her draft report transferred to improve her writing in general that she made use with her assignments.
Impact on the Falls Prevention Team
The team praised Renuka for her work and were enthusiastic to implement our recommendations for improving practice, these included changes in the ways they collected data and the inclusion of some behavioural change techniques to increase adherence. The following week we received an email confirming the changes made. It was rewarding to see our work had led to a direct, immediate, and practical, societal impact.
We can recommend the scheme as it provided an opportunity to co-create with the student and an NHS team that has led to a positive outcome that we hope in time will be shown to improve patient care. It also gave new insights into the factors that facilitate implementation of changes in an NHS team.
Dr Samuel Nyman and Louise Fazakarley
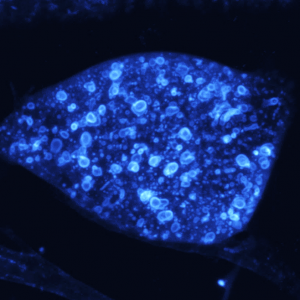 esearch, (led by me, Dr Paul Hartley), was recognised at UK Kidney Week in Liverpool last week. We were invited to speak about our fruit fly model of human renal disease, work that has been variously supported by grants from the British Heart Foundation and Kidney Research UK. The conference was an excellent opportunity to showcase the model and highlight our current collaborations with consultant-scientists based at Great Ormond Street Children’s Hospital as well as a number of different groups at the University of Bristol, the University of Osnabruck in Germany, Harvard Children’s Hospital and the University of Edinburgh. The research work is based in Dorset House labs and is supported by a wide network of talented people within BU as well as our undergrad and post-grad students.
esearch, (led by me, Dr Paul Hartley), was recognised at UK Kidney Week in Liverpool last week. We were invited to speak about our fruit fly model of human renal disease, work that has been variously supported by grants from the British Heart Foundation and Kidney Research UK. The conference was an excellent opportunity to showcase the model and highlight our current collaborations with consultant-scientists based at Great Ormond Street Children’s Hospital as well as a number of different groups at the University of Bristol, the University of Osnabruck in Germany, Harvard Children’s Hospital and the University of Edinburgh. The research work is based in Dorset House labs and is supported by a wide network of talented people within BU as well as our undergrad and post-grad students.


































 REF Code of Practice consultation is open!
REF Code of Practice consultation is open! BU Leads AI-Driven Work Package in EU Horizon SUSHEAS Project
BU Leads AI-Driven Work Package in EU Horizon SUSHEAS Project Evidence Synthesis Centre open at Kathmandu University
Evidence Synthesis Centre open at Kathmandu University Expand Your Impact: Collaboration and Networking Workshops for Researchers
Expand Your Impact: Collaboration and Networking Workshops for Researchers Visiting Prof. Sujan Marahatta presenting at BU
Visiting Prof. Sujan Marahatta presenting at BU ECR Funding Open Call: Research Culture & Community Grant – Apply now
ECR Funding Open Call: Research Culture & Community Grant – Apply now ECR Funding Open Call: Research Culture & Community Grant – Application Deadline Friday 12 December
ECR Funding Open Call: Research Culture & Community Grant – Application Deadline Friday 12 December MSCA Postdoctoral Fellowships 2025 Call
MSCA Postdoctoral Fellowships 2025 Call ERC Advanced Grant 2025 Webinar
ERC Advanced Grant 2025 Webinar Update on UKRO services
Update on UKRO services European research project exploring use of ‘virtual twins’ to better manage metabolic associated fatty liver disease
European research project exploring use of ‘virtual twins’ to better manage metabolic associated fatty liver disease