
RDS NEWS
From the RDS desk – navigating the innovation pathway
The RDS blog this month provides a few tips on putting together an i4i application Read the blog here
NIHR News
Major new funding opportunity for local government based public health research collaborations
eBulletins and Newsletters
NIHR Funding and support news: September 2021
NHS England and NHS Improvement: In Touch
Events
HEE SW NIHR Integrated Clinical Academic Awards Showcase Event
Online – MS Teams: Monday 20th September 2021 1.30pm – 2.30pm.
The event is open to everyone interested in finding out more about the awards. It will include:
- an introduction to the HEE-NIHR Integrated Clinical Academic programme and South West region awards from the HEE SW NIHR Programme Delivery Team
- presentations from previous awardees including an intern, pre-doctoral and postdoctoral awardees in the region.
- a Q&A session
Join on your computer or mobile app: Click here to join the meeting
Funding Opportunities
Latest NIHR funding calls
Transforming care and health at home and enabling independence
Public Health Research (PHR) Programme
NIHR Health Determinants Research Collaborations (HDRC)
Health Technology Assessment (HTA) Programme
21/554 Health Technology Assessment Programme Researcher-led (primary research)
21/555 Health Technology Assessment Programme Researcher-led (evidence synthesis)
21/556 NIHR NICE Rolling Call – (HTA Programme)
Your local branch of the NIHR RDS (Research Design Service) is based within the BU Clinical Research Unit (BUCRU) should you need help with your application. We advise on all aspects of developing an application and can review application drafts as well as put them to a mock funding panel (run by RDS South West) known as Project Review Committee, which is a fantastic opportunity for researchers to obtain a critical review of a proposed grant application before this is sent to a funding body.
Contact us as early as possible to benefit fully from the advice
Feel free to call us on 01202 961939 or send us an email.


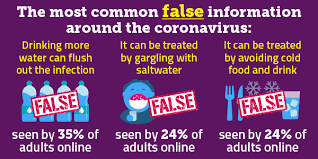
 Research at Bournemouth University is looking at the effectiveness of comic artistry and storytelling in the sharing of public health messaging.
Research at Bournemouth University is looking at the effectiveness of comic artistry and storytelling in the sharing of public health messaging.























 SPROUT: From Sustainable Research to Sustainable Research Lives
SPROUT: From Sustainable Research to Sustainable Research Lives BRIAN upgrade and new look
BRIAN upgrade and new look Seeing the fruits of your labour in Bangladesh
Seeing the fruits of your labour in Bangladesh Exploring Embodied Research: Body Map Storytelling Workshop & Research Seminar
Exploring Embodied Research: Body Map Storytelling Workshop & Research Seminar Marking a Milestone: The Swash Channel Wreck Book Launch
Marking a Milestone: The Swash Channel Wreck Book Launch ECR Funding Open Call: Research Culture & Community Grant – Application Deadline Friday 12 December
ECR Funding Open Call: Research Culture & Community Grant – Application Deadline Friday 12 December MSCA Postdoctoral Fellowships 2025 Call
MSCA Postdoctoral Fellowships 2025 Call ERC Advanced Grant 2025 Webinar
ERC Advanced Grant 2025 Webinar Update on UKRO services
Update on UKRO services European research project exploring use of ‘virtual twins’ to better manage metabolic associated fatty liver disease
European research project exploring use of ‘virtual twins’ to better manage metabolic associated fatty liver disease