The Allied Health Professions (AHPs) are the third largest clinical workforce in the NHS and represent a total of 14 professions which are regulated by the Health Care Professions Council and the individual profession specific regulatory bodies. Research is supported nationally and regionally through the Council for Allied Health Professions Research and at BU through our partnership collaboration with the Applied Research Collaboration NIHR Wessex.
To celebrate the 4th Annual AHP day at BU we are showcasing some of the research that is being carried out by the AHP academic community in Dorset.
Dr Katie Collins – Research focuses on the hidden impairments following a stroke and how they impact on individuals participating in active life. I am involved in exploring health equity and the impacts of health inequality and supervising a Dorset Health Care University Foundation Trust (DHCFUT): BU match funded PhD studentship exploring interventions for successful contracture management.’
Dr Vikram Mohan – Current project which has QR funding is aimed at exploring the reliability and validity of the Total Faulty Breathing Scale (TFBS). In clinical practice abnormal breathing patterns are recognised, but there are no scales to quantify the severity of abnormal breathing patterns. These findings will be applied to conditions like Covid-19, COPD etc.
Peter Philips – PhD – “What factors affect resilience in newly qualified paramedics in the UK ambulance service?” Aims to explore stressors that newly qualified paramedics face in their first year of registration, how they seek to cope with those stressors, and what effect these have. This research will have an impact on workforce planning, recruitment, and retention of staff in the NHS.
Helen Ribchester – PhD- Exploring sense making derived from the clinical practice experiences of student Occupational Therapists in India. An This is an IPA study including elements of poetic inquiry, with participants drawn from the students of an occupational therapy programme in an Indian university (SRIHER)
Sara Sayer and Prof Carol Clark – ‘Heading for Trouble’ project, with pump prime funding, involving external stakeholders and an interdisciplinary team from the Faculty of SciTec (Prof Hamid Bouchachia, Prof Hana Burianova, Dr Ala Yankouskaya, Dr Shanti Shankar) aiming to explore brain scans and questions relating to attention and memory in professional footballers. Supporting health in football.
Dr Theo Akudjedu and Dr John Totman – working within the Institute for Medical Imaging and Visualisation (IMIV) a multidisciplinary collaboration of clinicians and scientists using a Siemens 3T MRI scanner for research projects to image liver, pancreatic and biliary disease and the brain.
Dr Ursula Rolfe – co-published with David Partlow a paramedic colleague from practice – Mental Health Care in Paramedic Practice The book provides paramedics with key information on a range of mental health conditions and their management. The roles of paramedics have changed in the last decade with increases in the number of 999 calls associated with the increasing mental health needs of people.
Dr Louise Fazakarley, Dr Katie Collins and Dr Caroline Ellis-Hill – supervising a funded MRes Carrie Tbaily ((DHCFUT) – Exploring caregiver perspectives of adults with severe and profound and multiple Learning disabilities accessing sedentary hydrotherapy.
Dr Louise Fazakarley – Pump prime funding to; examine the effectiveness of Physiotherapy in the early stage of Parkinson’s disease (PD): a review of the literature and Patient and Public Involvement (PPI) consultation to identify research priorities for patients with early-stage PD
Sam Page (Dorset County Hospital (DCH)), Dr Louise Fazakarley and Dr Zoe Sheppard (DCH) -ARC Wessex NIHR funding to undertake a service evaluation relating to patients who sustain pubic rami fracture and their management at home supporting better care for patients.
Dr Caroline Ellis-Hill – research focus is on humanising practice, based on existential understandings from lifeworld approaches and focuses on what make us feel human. Humanising practices are those that incorporate fully human knowing and support a sense of connection and wellbeing. Caroline has funding from the Welcome Trust – Exploring performance arts education for the stroke rehabilitation pathway, is supervising PhD students as part of the INNOVATEDIGNITY project funded by the European Commission and NIHR funding for a multicentre RCT of community-based arts and health intervention to increase psychological wellbeing in people following stroke.
Prof Carol Clark – supervising Rosie Harper (University Hospitals Dorset (UHD) with Dr Carly Stewart (BUBS) and Sally Sheppard (UHD) on a UHD; ARC Wessex NIHR; BU match funded studentship ‘Nudging: a theoretical concept for a very practical approach to pelvic floor muscle training’ Aimed at improving adherence to exercises aimed at reducing incontinence and improving health and well-being of women. Carol is currently Co-PI with Stefi Andrew (Portsmouth Hospitals University Trust) and Dr Zoe Sheppard (DCH)on NIHR ARC Wessex Exploring digital technologies for hand rehabilitation and Danni Swaithe (UHD), Dr Louise Johnson (UHD) Dr Shanti Shankar (SciTech) NIHR ARC Wessex, exploring the role of attentional focus on learning for physical recovery in acute stroke, research initiation award.
Prof Jane Murphy Co-Lead of the Aging and Dementia Research Centre current project includes NIHR ARC Wessex funded, DONOR project (Digital cOachiNg fOr fRailty) to investigate whether a digital approach could be used alongside support from health coaches to help the lifestyle management of older people with frailty in its early stages. The DONOR project will look at whether these technologies can reduce the burden on health and care services by offering person-centred care and advice. The multidisciplinary research team will work together with stakeholders (people with frailty, carers, health coaches and AHPs) to develop and test a new digital approach, implemented across Dorset and West Hampshire. Jane provides consultancy services, works with the Wessex Academic Health Science Network and International partners and also has funding as part of the ASPIRE project with European funding.
Dr Jonathan Williams – is currently involved in projects broadly investigating clinical and sports biomechanics, including wobble board rehabilitation for diabetic neuropathy; learning and retention of infant CPR skills, quantifying spinal stiffness and movement through body worn sensors; facilitating physical activity through wearables; measurement of player load in Badminton and shoulder sensory-motor control. He is currently supervising MRes and PhDs projects with AHPs including Andy Watt and Debora Almeida.
Debora Almeida PhD – A novel output-based approach to infant CPR training to maximise skill retention and improve patient outcome after cardiac arrest. Paediatric cardiac arrest is a worldwide health problem with high rates of morbidity and mortality. Positive outcomes depend on high quality CPR. However, infant CPR skills decay within weeks or months after training. This project aims to create a tailored retraining schedule based on the performance and retention of iCPR skills.

 The
The 






 gland ) Project Output (supporting mental health and wellbeing in India)
gland ) Project Output (supporting mental health and wellbeing in India) 
 Kate Adie, broadcaster, author and the University’s fifth Chancellor is familiar with sites of conflict and destruction. In her introduction to the
Kate Adie, broadcaster, author and the University’s fifth Chancellor is familiar with sites of conflict and destruction. In her introduction to the  morate Mass Graves Day in Iraq, the International Commission on Missing Persons (ICMP) presented the recently published Bournemouth Protocol on Mass Grave Investigation and Protection to Iraqi authorities involved in efforts to account for missing persons.
morate Mass Graves Day in Iraq, the International Commission on Missing Persons (ICMP) presented the recently published Bournemouth Protocol on Mass Grave Investigation and Protection to Iraqi authorities involved in efforts to account for missing persons.















 New weight change BU paper
New weight change BU paper One week to go! | The 16th Annual Postgraduate Research Conference
One week to go! | The 16th Annual Postgraduate Research Conference Geography and Environmental Studies academics – would you like to get more involved in preparing our next REF submission?
Geography and Environmental Studies academics – would you like to get more involved in preparing our next REF submission? Congratulations to three former BU staff
Congratulations to three former BU staff Applications are now open for 2025 ESRC Postdoctoral Fellowships!
Applications are now open for 2025 ESRC Postdoctoral Fellowships! Horizon Europe – ERC CoG and MSCA SE webinars
Horizon Europe – ERC CoG and MSCA SE webinars ERC grants – series of webinars
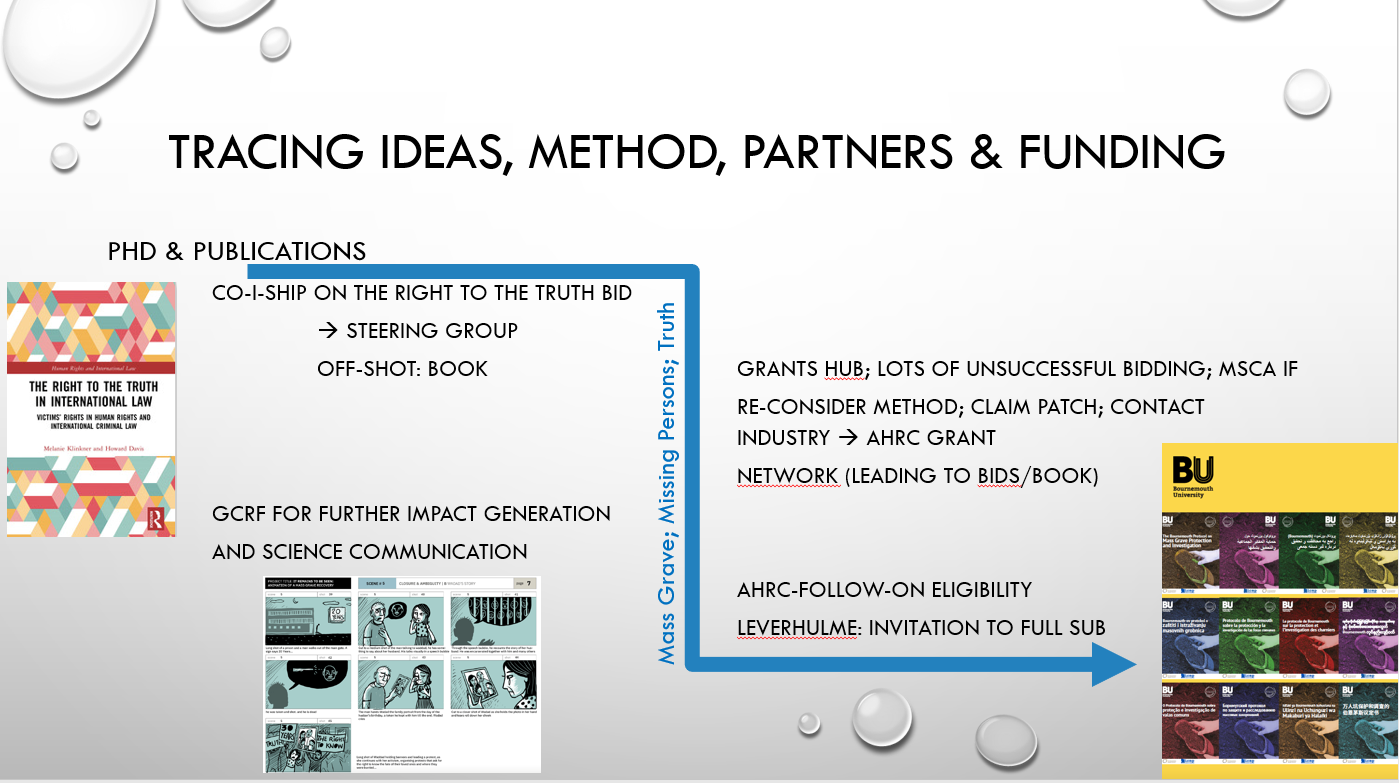
ERC grants – series of webinars MaGMap: Mass Grave Mapping
MaGMap: Mass Grave Mapping Last reminder – MSCA Postdoctoral Fellowships 2024 internal deadline next week
Last reminder – MSCA Postdoctoral Fellowships 2024 internal deadline next week